Arthritis of the Knee
Arthritis is inflammation of one or more of your joints. Pain, swelling, and stiffness are the primary symptoms of arthritis. Any joint in the body may be affected by the disease, but it is particularly common in the knee.
Knee arthritis can make it hard to do many everyday activities, such as walking or climbing stairs. It is a major cause of lost work time and a serious disability for many people.
The most common types of arthritis are osteoarthritis and rheumatoid arthritis, but there are more than 100 different forms. While arthritis is mainly an adult disease, some forms affect children.
Although there is no cure for arthritis, there are many treatment options available to help manage pain and keep people staying active.
Anatomy
The knee is the largest and strongest joint in your body. It is made up of the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). The ends of the three bones that form the knee joint are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones as you bend and straighten your knee.
Two wedge-shaped pieces of cartilage called meniscus act as “shock absorbers” between your thighbone and shinbone. They are tough and rubbery to help cushion the joint and keep it stable.
The knee joint is surrounded by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage and reduces friction.
Description
Osteoarthritis
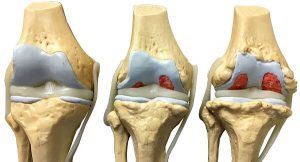
Osteoarthritis is the most common form of arthritis in the knee. It is a degenerative, wear-and-tear type of arthritis that occurs most often in people 50 years of age and older, although it may occur in younger people, too.
In osteoarthritis, the cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone and produce painful bone spurs.
Osteoarthritis usually develops slowly, and the pain it causes worsens over time.
Osteoarthritis often results in bone rubbing on bone. Bone spurs are a common feature of this form of arthritis.
Posttraumatic Arthritis
Posttraumatic arthritis is form of arthritis that develops after an injury to the knee. For example, a broken bone may damage the joint surface and lead to arthritis years after the injury. Meniscal tears and ligament injuries can cause instability and additional wear on the knee joint which, over time, can result in arthritis.
Symptoms
A knee joint affected by arthritis may be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There are other symptoms, as well:
- The joint may become stiff and swollen, making it difficult to bend and straighten the knee.
- Pain and swelling may be worse in the morning, or after sitting or resting.
- Vigorous activity may cause pain to flare up.
- Loose fragments of cartilage and other tissue can interfere with the smooth motion of joints. The knee may lock or stick during movement. It may creak, click, snap, or make a grinding noise (crepitus).
- Pain may cause a feeling of weakness or buckling in the knee.
- Many people with arthritis note increased joint pain with changes in the weather.
Physical Examination
During the physical examination, your doctor will look for:
- Joint swelling, warmth, or redness
- Tenderness around the knee
- Range of passive (assisted) and active (self-directed) motion
- Instability of the joint
- Crepitus (a grating sensation inside the joint) with movement
- Pain when weight is placed on the knee
- Problems with your gait (the way you walk)
- Any signs of injury to the muscles, tendons, and ligaments surrounding the knee
- Involvement of other joints (an indication of rheumatoid arthritis)
Imaging Tests
- X-rays.These imaging tests provide detailed pictures of dense structures, such as bone. They can help distinguish among various forms of arthritis. X-rays of an arthritic knee may show a narrowing of the joint space, changes in the bone, and the formation of bone spurs (osteophytes).
- Other tests.Occasionally, a magnetic resonance imaging (MRI) scan or a computerized tomography (CT) scan may be needed to determine the condition of the bone and soft tissues of your knee.
Treatment
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability it can cause.
Nonsurgical Treatment
As with other arthritic conditions, initial treatment of arthritis of the knee is nonsurgical. Your doctor may recommend a range of treatment options.
Lifestyle modifications. Some changes in your daily life can protect your knee joint and slow the progress of arthritis.
- Minimize activities that aggravate the condition, such as climbing stairs.
- Exercise is recommended for osteoarthritis to improve pain and function. Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will enable you to be active while putting less stress on your knee. Balance, agility, and coordination exercises, combined with traditional exercise, may help to improve function and walking speed.
- Losing weight can reduce stress on the knee joint, resulting in less pain and increased function.
Exercises for arthritis
Exercises for arthritis might include exercises that put joints through their full range of motion and strengthening exercises. Exercise that raises heart rate, known as aerobic exercise, is also important.
Range-of-motion exercises
These exercises lessen stiffness and put joints through their full range of motion. Examples of these exercises are stretching arms up high or rolling shoulders forward and backward. Most of these exercises can be done every day.
Strengthening exercises
These exercises help build strong muscles that can support and protect the joints. Weight training is an example of exercise that can help build and keep muscle strength. Using resistance bands, hand weights or machines can help build strength.
Weight training should be done every other day for at least two days a week. It should include all the major muscles in the body.
Aerobic exercise
Exercises that raise heart rate, known as aerobic exercises, help with overall fitness. They can improve heart and lung health, help control weight, and increase energy.
Examples of aerobic exercises that are easy on joints include walking, bicycling, swimming and water aerobics. Try to work up to 150 minutes of somewhat hard aerobic exercise every week. You can exercise 10 minutes at a time if that’s easier on your joints.
It’s best to do moderate aerobic activity most days of the week. But even a couple of days a week can help. Exercise at a rate at which breathing is harder than usual while still being able to talk.
Other activities
Any movement, no matter how small, can help. Daily activities such as mowing the lawn, raking leaves and walking the dog count.
Exercises that focus on how the body moves, such as gentle forms of yoga or tai chi, also can help. They can improve balance and posture, prevent falls, and ease tenseness.
If you’re in an exercise class, tell your teacher about your arthritis. Listen to your body. Don’t do anything that causes pain.
Tips to protect your joints
If you haven’t exercised in a while, start slowly. Don’t push yourself too hard — that can overwork muscles and make joint pain worse.
Consider these tips:
- Keep the impact low.Low-impact exercises help keep joint stress low while you move. Examples include stationary or recumbent bicycling, elliptical trainer workouts, or exercise in the water.
- Use heat.Heat can relax joints and muscles and lessen pain before exercise. Deliver the heat with warm towels, hot packs or a shower. The temperature should be warm, not painfully hot. Use for about 20 minutes.
- Move gently.Move joints gently at first to warm up. You might begin with range-of-motion exercises for 5 to 10 minutes before you move on to strengthening or aerobic exercises.
- Go slowly.Exercise with slow and easy movements. If you feel pain, take a break. Sharp pain and pain that’s worse than the usual joint pain might mean something is wrong. Slow down if you see swelling or redness in your joints.
- Ice afterward.Use ice on your joints for up to 20 minutes as needed after activity. This is even more important if your joints are swollen.
Listen to your body. Don’t push too hard. Build up slowly. Add more and harder exercise as you get stronger.
Singh Snapshot
Many people believe that running causes knee osteoarthritis (OA), but doctors now know this isn’t true. Researchers who compared long-term effects of running and other strenuous forms of exercise found that running significantly decreased the risk of hip and knee replacement, while some other forms of exercise increased it. Another long-term study showed that the incidence of hip and knee OA was three times higher in sedentary people than in recreational runners. Elite competitive runners, on the other hand, had more cases of hip and knee OA than people who didn’t exercise.





Leave a Reply